Latests posts by FINAOStarterAdmin
Health insurance disruption is killing the legacy core system
Health Core Systems

7 Trends in insurance claims management 2023
Claims Management

Why personalization is critical for growing health insurers
Health

Transitioning from legacy systems to modern insurtech platforms
Insurtech Core Systems
What is insurance management software?
Insurtech

Why policy admin systems need an upgrade
Policy Administration

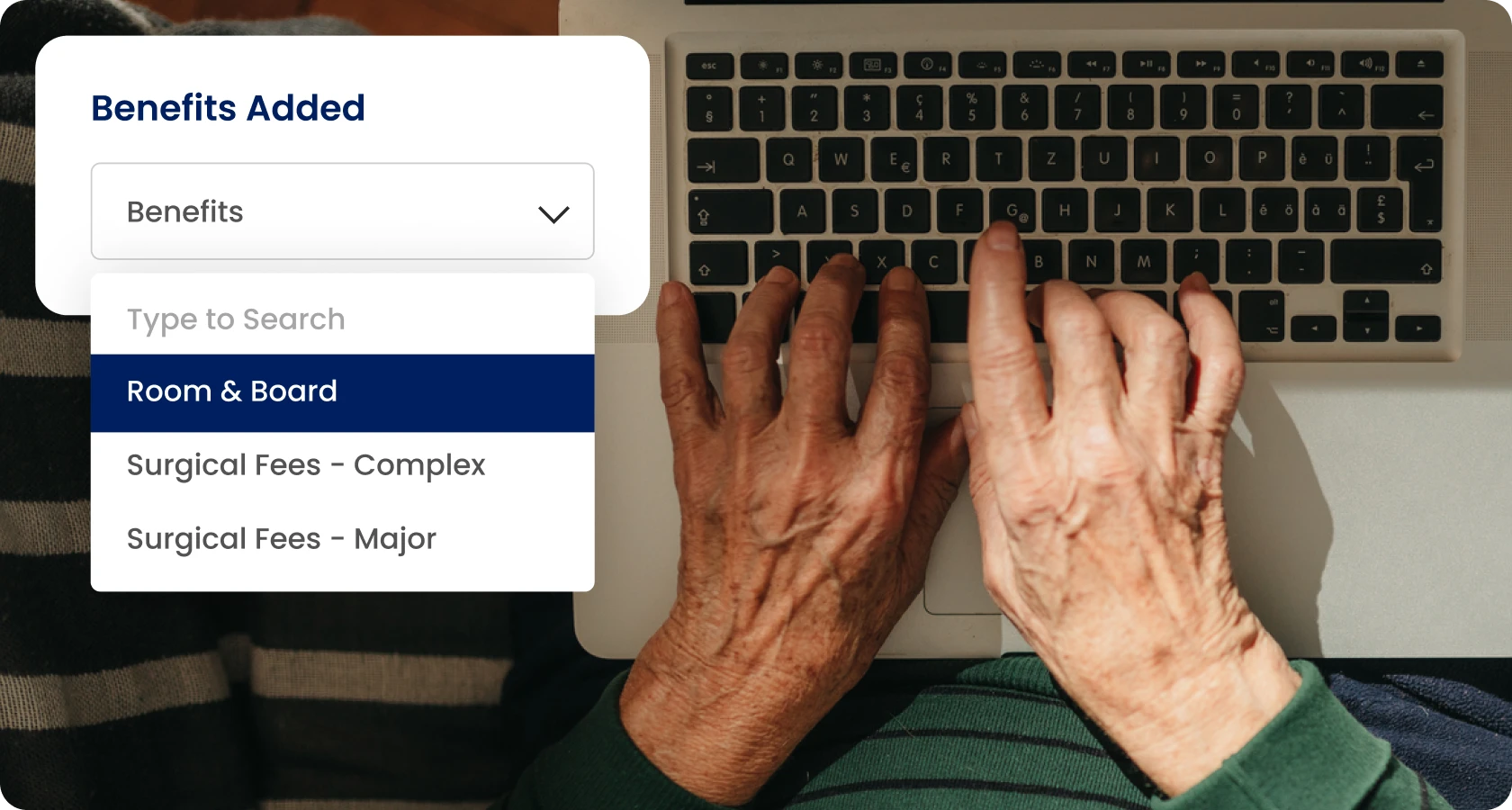
Why health insurers need better product flexibility
Health

Should insurers integrate with insurtech platforms?
Insurtech
Why old-school thinking is holding back the insurance industry
Insurtech

Why customer experience is crucial for health insurers
Health

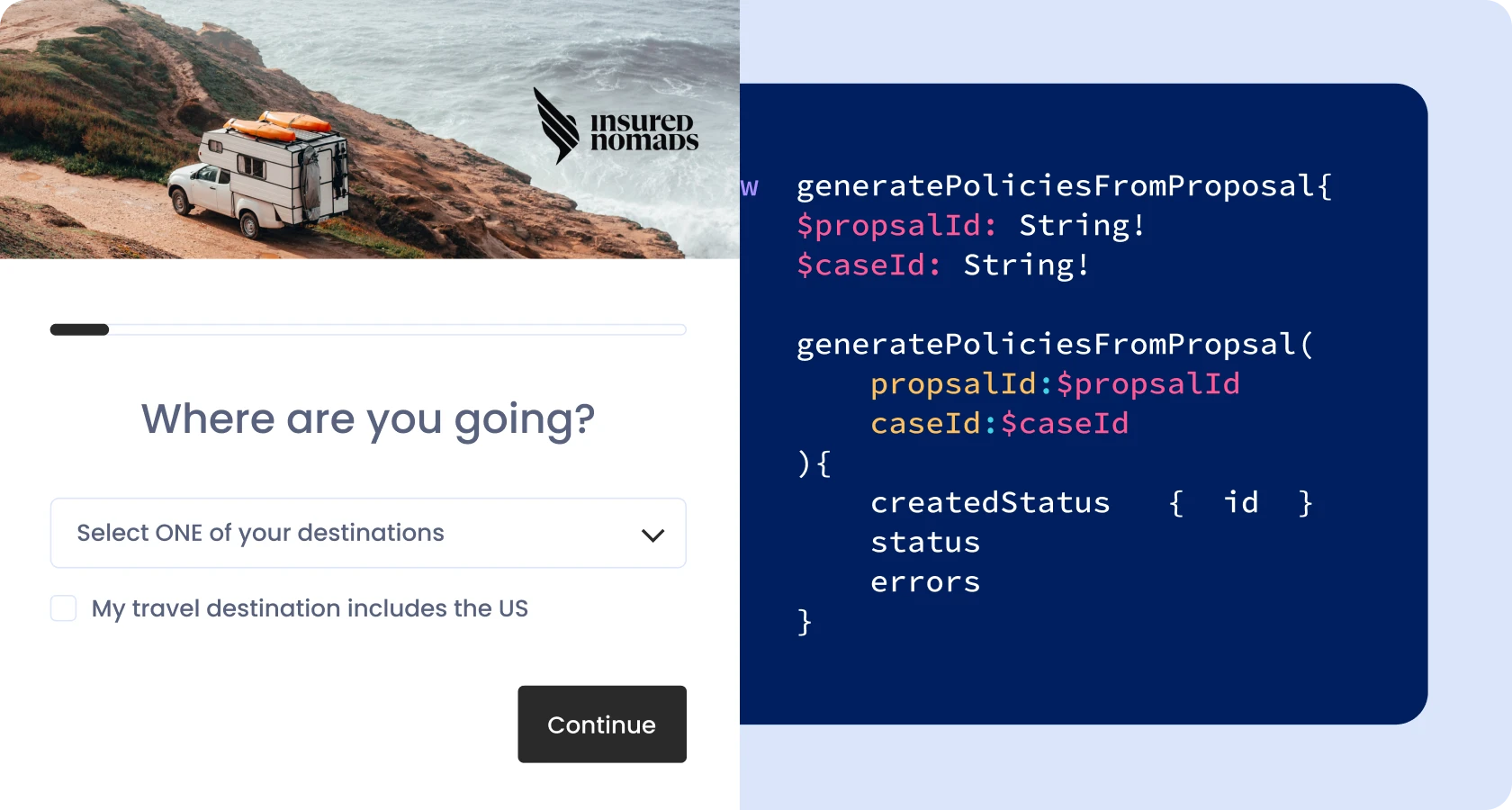
The Role of APIs in the digitalization of insurance companies
Insurance APIs
10 Ways to improve insurance claims processes
Claims Management
